Executive Summary
- Testing for COVID-19 involves examining secretions from the nose and mouth for genetic material from the virus using a technique called polymerase chain reaction (PCR).
- It is very effective at identifying who is actively shedding virus and thus can infect others.
- It will not identify who has been infected, who is infected but not yet shedding virus or who has been infected and is no longer shedding virus or shedding low levels of virus. Therefore it won’t tell us the prevalence of COVID-19, or how many people have been infected.
- Therefore, viral testing should not replace or limit social distancing or other control measures.
People have been making statements about testing for COVID-19 that are inaccurate and confusing. I write this post to clarify the role of testing for the virus in controlling the pandemic and to explain the confounding issues with any tests for this purpose. Remember, designing any new test, validating it, scaling it up for millions of people and making sure the people that collect the samples and run the test don’t get infected is a logistic nightmare. Even Dominos would have a nearly impossible task if they set up new nationwide pizza ordering, preparation and deliver system while making sure everyone gets the pizza they ordered (and cooked the way they want) while ensuring the safety of delivery in a matter of weeks! A new testing system for corona virus is as great a challenge, especially since it has been less that 3 months since the virus was reliably identified.
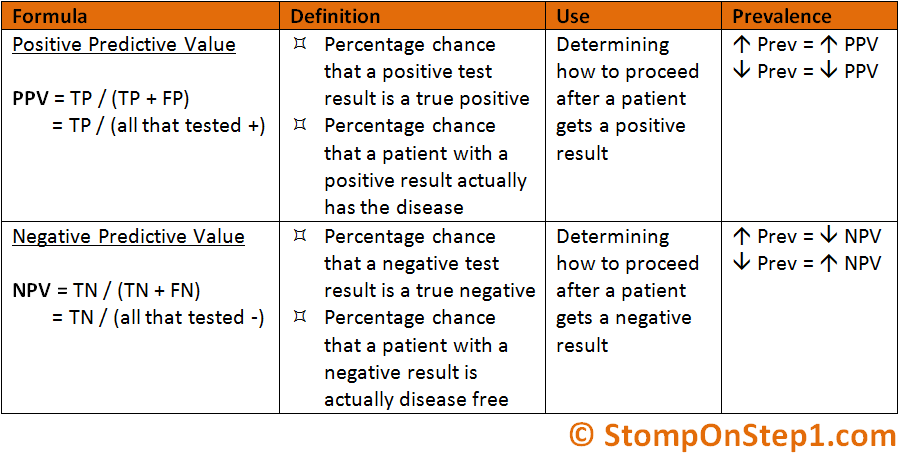
First some background. We test individuals to find out who’s infected with COVID-19 so we can isolate them and prevent the spread of the virus. This sounds simple, but is actually complex. The ability of any test to identify infective individuals is called the POSITIVE PREDICITVE VALUE of a test.
(see https://en.wikipedia.org/wiki/Positive_and_negative_predictive_values)
This means the ability of a test to tell people who are truly infected (true positives) from people who come up positive but not infected (false positives). This ability to discriminate infected people can only come from evaluating the test on people known to be infected. It is somewhat circular, but you can’t tell how good your test is until you test it!
So initially to prove the value of a test it must first be evaluated on people who had the virus grown in tissue culture from their nose or lungs during infection. In the case of corona virus, those studies were done in populations in Asia and in Europe, where the number of infected people was relatively high (high prevalence). As shown in Equation 1, higher prevalence makes any test look better. In contrast where the number of infected people is low any test works less well because there are fewer infected people (true positives) to false positives. Different populations also can have more false negative tests for other reasons, such as changes in the virus (RNA viruses mutate rapidly) or less viral shedding from prior exposures to related viruses. Because of this the CDC wanted to validate the COVID-19 test for the United States population. The speed of this pandemic made that impossible and tests validated on other populations are now being used in the US. This attempt to customize the test for the US was a legitimate effort but was overwhelmed by circumstances. This is still a concern however, since only 1% of patients are testing positive in the US, which may lead to a significant number of false positives (although quarantining uninfected people has little down side).
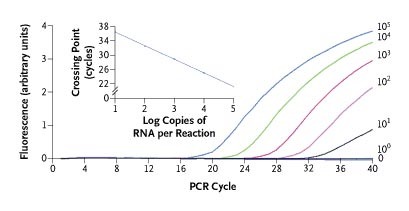
A major issue is the type of test is being used. All current COVID-19 testing is based on polymerize chain reaction (PCR) amplification and identification of viral RNA from swabs of the nares and throat. What this testing does is make copies of COVID-19 specific RNA and label them with a fluorescent dye. The fluorescence is then detected and quantified. A person is only “positive” when the virus is growing and RNA is being produced. This is useful in identifying people that actively producing virus so that they can be isolated and not infect others. However, it doesn’t identify anyone who has recently been affected and has eliminated the virus, is infected but has not yet produced the virus, or maybe in the recovery phase and only transiently produces virus. You can see this in Figure 3 where the patient was infected for several days before the PCR test became positive, then was negative in the lungs and nares while still shedding virus in the stool.

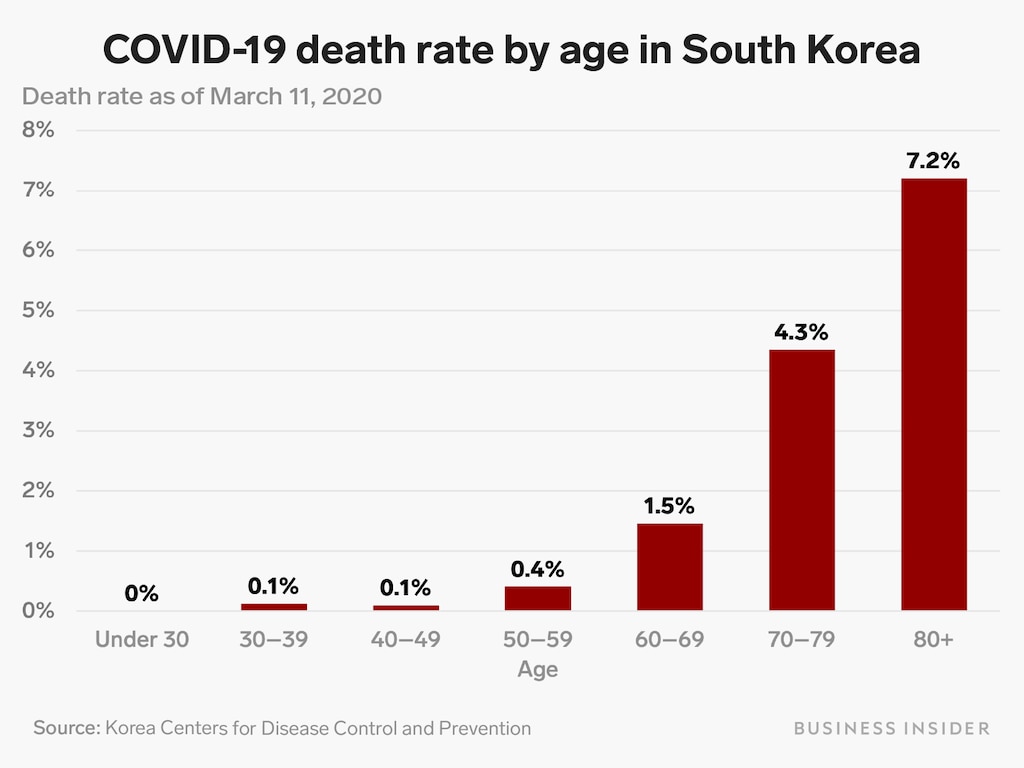
Since people who were previously infected are not identified by this test, it also means that the testing doesn’t give any type of information about the extent of infection in the entire population. This is particularly important when people make statements about the “mortality rate” or deaths per number of people infected with COVID-19. This is important as higher death rates suggest the infection could overwhelm our health system. While death rate numbers have been touted from 1-9%, currently there is no way to tell what the mortality rate is from this virus because we don’t know how many the people have been infected. In South Korea, which has had one of the most extensive PCR testing programs, death rates have been very low in individuals below 70 and without heart or lung disease (Figure 3) and rates are likely to be even lower if all prior infections are considered. This it is important to be careful when evaluating the reported death rate from this infection
Finally, you only want to be screened for this infection if you truly have symptoms. Any test is only as good as the likelihood of picking up a positive. In the low frequency populations, the likelihood of a true positive infection is very low and therefore the likelihood of a positive false-positive reaction is fairly high in comparison. Even now only 1% of the patients screen for coronavirus are coming a positive; most of the people have other types of colds, of the flu or infections. Therefore, you only increasing the likelihood of a false positive reaction unless you have symptoms compatible with coronavirus infection.
I hope this information helps clarify the issues surrounding screening test for COVID-19 and allows you to dismiss many of the things are being said on TV about death rates or infection rates. We just don’t know those numbers and while I think it’s good to take precautions such as social distancing we won’t know exactly how many people will get sick for several weeks.
So, prepare for the worst and hope for the best.
Great Article. Just last night we were talking about the issues addressed here and that the government was not dealing with in their somewhat ridiculous daily press conferences. People are not so stupid that they cannot deal with true and meaningful facts. Thank you Mr Baker!
I have a question though about what I read lately regarding “cure” of the virus using chloroquine or Lopinavir/Ritonavir. Although it seems that the attempt to use those drugs started in China with apparently some success, they have been used with success in Australia and France by reputable research centers. Can you elaborate on this in one of your blog? I realise that it is not a prevention like a vaccine. But in the meantime at least it could help some patients. Thanks.
LikeLike
Please comment on the “herd immunity” concept. Thank-you!
LikeLike
Herd immunity is the protecting provided to a non-vaccinated person by other who are vaccinated and can infect
LikeLike
swabs of the nares and throat.
what is a “nare”? I suspect you meant “nose”?
LikeLike
yes. term for one of the nose “holes”
LikeLike